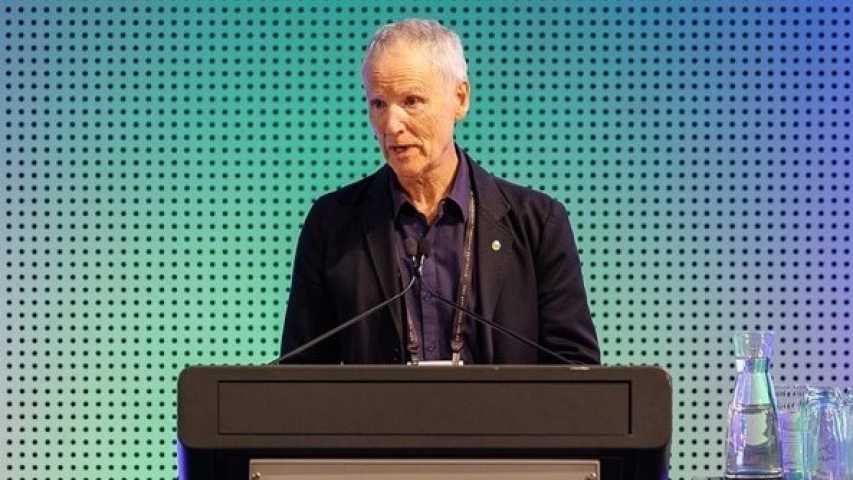
By Dr Antoinette Anazodo, Paediatric and Adolescent Oncologist at Sydney Children's Hospital and Prince of Wales Hospital, Director of The Sydney Youth Cancer Service, Churchill Fellow 2015.
Since beginning my career in paediatric and adolescent oncology, it’s been my goal to amplify the voices of young cancer patients. I’ve been particularly focused on fertility, which always strikes a chord with me when Mother’s Day rolls around each year.
We know that when young people are diagnosed with cancer, the specialist teams responsible for their care, such as the Youth Cancer Services, become a vital part of their journey. But what people don’t realise is that these teams focus on ALL aspects of that young person’s life, including what the future could look like for them if they want to become parents.
I’ve always thought it really tough that young people as young as 13 have to think about whether they want to freeze their eggs or sperm. Most people start to think about starting a family a decade later, sometimes two. Unfortunately though, these conversations around cancer treatment and its effect on fertility don’t always happen.
That’s why I’m proud to have been involved in a 12-year evaluation of the reproductive complications for cancer survivors led by the Kids Cancer Centre. What my colleagues and I found is that these young people have multiple ongoing reproductive concerns that change over time. This means that it’s never been more important to ensure that current models of cancer care routinely have reproductive follow-up conversations to help young people explore their best chance at parenthood.
On the flip side, when these conversations around fertility don’t happen for young cancer patients, it can take a toll later in life as they approach parenting age. Social concerns and expectations surrounding infertility have been shown to have a negative impact on the quality of life of young people who have had cancer. Again – another critical reason to arm young cancer patients and survivors with specialist support and information. This avenue has the potential to improve a young person’s quality of life because they’re then better able to manage their infertility-related social concerns and improve their acceptance of illness.
If you have a spare five minutes, I encourage you to read this piece in the Sydney Morning Herald which features an incredible young person called Sophie. Even though it was first published around three years ago, the sentiment Sophie brings, and the way she talks about her ongoing survivorship journey, will really bring this issue to life for you.
Finally, over the past few years, I’ve been more and more aware of conversations around sexuality and cancer treatment. Sexuality and fertility to me are both very connected and very separate. I think what’s hard for young people is that there is so much going on in those teenage years that finding their way through either or both of these things, and adding a cancer diagnosis into the mix, is something that we absolutely need to help them through so they don’t feel invisible or like they’ve fallen through the cracks.
There’s a fantastic resource available for LGBTIQ+ young cancer patients developed by our friends at the ONTrac at Peter Mac Victorian Adolescent and Young Adult Cancer Service if you or someone you know needs this type of support and guidance.
Canteen also has two books (available to read online too), called Maybe later baby? They’re a wonderful entry point to relationships, sex and fertility for both young people with cancer and what can happen after cancer.